Lamellar keratoplasty is a surgical technique developed to replace one or more of the five corneal layers, but not the whole cornea.
Keratoplasty is the replacement of a damaged cornea with a donor transplant. In lamellar keratoplasty, the healthy and clear portions of the recipient’s own cornea are preserved, significantly decreasing surgical trauma and the chance developing host-versus-graft disease. In anterior lamellar keratoplasty, the inner layers of the cornea (Descemet’s membrane and corneal endothelium) are preserved. This technique significantly extends the life span of the transplanted cornea (to up to 49 years).
This procedure is very precise, limited to removing a tissue fragment of up to 300-500 microns in thickness. This very delicate method requires high-tech equipment and special surgical skills. Trephination devices with micrometre scales or femtosecond laser systems are needed to perform the surgery.
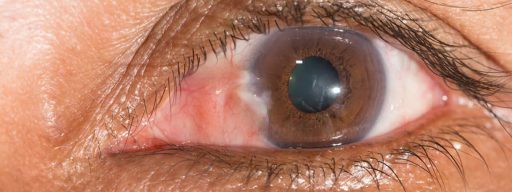
Cornea diseases is the fourth-most common cause of blindness in the world population. Corneal transplantation is also the only way to restore vision in cases of severe cornea opacifications.
Anterior lamellar keratoplasty is indicated in:
- Keratoconus.
- Pellucid marginal degeneration.
- Some congenital hereditary corneal dystrophies.
- Superficial corneal scars of traumatic or inflammatory origin.

You can make an appointment by phone from 8:30 to 19:30 (daily).
In the following cases, corneal transplantation is strictly contraindicated:
- Lid abnormalities (entropion or ectropion). In entropion, the eye mucous membrane is constantly injured by the eyelashes; in ectropion, this membrane is exposed and subject to drying out.
- Blepharitis and blepharon-conjunctivitis, which are inflammatory processes affecting the eyelids and the mucous membrane of the eye.
- Active inflammatory processes of the eye.
- Severe systemic disorders.
The success of surgery depends on the correct diagnosis. The depth of corneal opacification should be accurately determined using special optical coherence tomography systems. It is also necessary to ensure the healthy condition of the posterior corneal layers before outlining the intervention plan.
Preoperative examination includes eye biomicroscopy, corneal topography, corneal tomography, keratometry, and biometry, as well as the assessment of the eye posterior segment.
In order to prevent postoperative complications, donor material (corneal transplant) is carefully selected and prepared. Surgical treatment can be carried out under general or local anaesthesia.
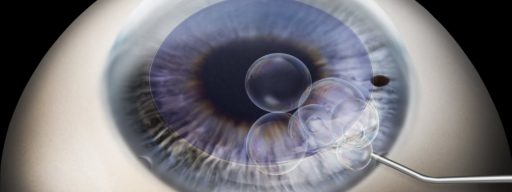
Lamellar keratoplasty consists of the following steps:
- Preparing patient for the surgery.
- Circular lamellar dissection of the outer layers of the cornea.
- Removal of the affected corneal tissue.
- Corneal transplant preparation.
- Transplant fixation in the donor bead using very fine sutures.
Anterior lamellar keratoplasty is a unique opportunity to restore vision in the case of various corneal pathologies.